Last updated on August 30th, 2022
One of the health problems due to improper control of diabetes is foot ulcers and foot pain. Every thirty seconds, someone loses a lower limb due to diabetes mismanagement. A leading cause of 85% of leg amputations in diabetic people is a bad foot ulcer. It is, therefore, necessary to know more about diabetic foot ulcers and foot pain causes and the best possible remedies.

What are Foot Ulcers?
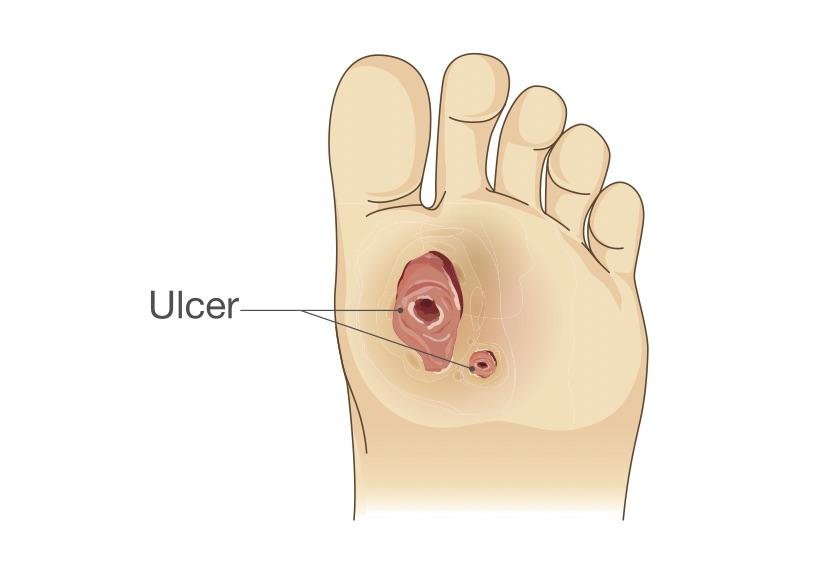
Foot ulcers are open sores that damage the outer skin and can expose the inner layers of the body. These may reach inner bones and can lead to serious issues like leg amputations if left untreated. Ulcers occur for different reasons, so determining the underlying medical problem that caused the ulcer is significant.
Also Read: Diabetic Diet Chart Indian

Symptoms of Foot Ulcers

Foot ulcers may look almost like a wound on the flesh of the foot. Key points about ulcer and their appearance:
- Pain: Ulcers may have no pain in the starting. But it can grow later and cause pain. It is pain that causes difficulty while walking.
- Dry and scaly area: Area near ulcer may have redness or dry or scaly skin.
- Itching: There may be a burning or itching sensation around ulcers.
- Change of color: The color of the ulcer varies on its type. It can be reddish-brown, yellowish, or brown-black.
- Fluid discharge: Some ulcers discharge fluids. Some ulcers may have a bacterial infection due to which they can give bad odors.
- Numbness: Some people complain of numbness around the ulcer it is due to poor circulation and nerve damage.
- Swelling: Some people may have unusual swelling around the leg and foot area.
Summary:
The symptoms of the foot ulcer are different from person to person. If you notice any change of skin color or a wound around the foot, consult the doctor.
Also Read: Normal sugar level fasting
Causes of Foot Ulcers

The cause of diabetic foot ulcers is mainly due to the following:
- Poor blood circulation
- Hyperglycaemia (high blood sugar levels)
- Lymphedema ( damage in lymphatic drainage system due to which there is swelling)
- Nervous damage
- Feet irritated or wounded
Due to vascular disease, the blood flow is not proper in the body. This results in poor blood circulation and results in leg swelling, blood clots, etc. These can cause ulcers in the inner part of the leg just below the knees.
A high glucose level in the blood slows down the body’s healing process due to which any small infection can turn out to be serious. People with type 2 diabetes are more vulnerable to foot ulcer infections.
Excess fluid in lymph causes swelling in nearby soft tissues of the leg and arms. This condition is called Lymphedema and can lead to fluid-filled ulcers. It can be painful and can become serious if left untreated.
Nerve damage can be due to diabetes or an injury and causes loss of sensation around the affected area. It has a long-term impact and can result in loss of sensation. Nerve damage reduces the sensitivity to foot pain due to which one can have painless foot ulcers.
Summary:
Diabetes, poor circulation, nerve damage, swelling in lymph, and improper diabetes management are causes of foot ulcers.
Also Read: How to reduce sugar level home remedies
Types of Foot Ulcers
Foot ulcers are classified based on the causes and are of four types:
Neuropathic: Also known as diabetic foot ulcers, these are red or brown. These occur when a patient’s feet lose sensation due to nerve damage. This ulcer is common in people with diabetes. It can also be due to be chronic alcohol consumption or nerve trauma. This ulcer is located in the high-pressure points of the feet.
Arterial: Poor blood circulation in the leg is the main cause of this type of ulcer. These ulcers are located on the heels, toes tips, or between the toes, and near the nail bed. These are yellowish or greyish.
Venous: Unusual functioning of the vein causes venous ulcers. Veins are blood vessels that carry impure blood from body organs to the heart. Due to injury, clots, aging, heavyweight the valves work improperly or may stop working. This causes fluid accumulation and thus swelling in the legs, and foot pain. Due to fluid accumulation, there may be fluid discharge. Swelling increases pressure around the leg due to which there is skin tear and it later develops into a foot ulcer. Generally, these foot ulcers are red.
Decubitus: Also known as pressure sores. Excessive foot pressure causes such ulcers. The high pressure causes a decrease in blood supply to the skin. This damages the tissues resulting in an open sore or wound.
Summary:
Diabetes, poor circulation, nerve damage, swelling in lymph, and improper diabetes management are causes of foot ulcers.
Also Read: zumba dance benefits
Treatment, Management & Guidelines

Treatment: People with diabetes have more risk of foot ulcers. Foot ulcers are the main reason for leg amputations (removal) worldwide. Immediately treating foot ulcers is therefore necessary. Treatment varies from person to person condition and this includes:
Medication: Medicine treatment includes:
- Antibiotics – to control infection of sore or wound
- Anticlotting medicines – to reduce blood clots and improve blood circulation
- Diabetic control medicines – to control diabetes.
- Painkillers – to relieve pain due to foot ulcers.
Surgical options: Surgery may include:
- Surgeries for increasing blood flow around the ulcer area by removing any bone deformities or by trimming the nearby bone.
- Regular debridement- Removal of infected tissues.
- Surgical revascularization – to improve blood flow to the infected area so the skin can heal properly.
Summary:
Foot ulcer treatment includes antibiotics and anti-clotting medicines, and it may require surgeries for increasing blood flow.
Management: Management of foot ulcers consists of providing relief from the ulcer pain or itching and to stop its growth. This includes:
- Wound offloading – is removing some weight or pressure from the wound to heal. Crutches or special footwear or braces are used in this case.
- Debridement is removing dead skin and tissue near the infected area.
- Compression Wraps: to reduce swelling below the knee area is wrapped with compression stockings or bandage.
- Specialized dressings- used for helping the skin near foot ulcer to heal. This may include antimicrobial dressing, collagen wound dressing, moist dressing, hydrogels dressing, based on the foot ulcer type.
- Hyperbaric oxygen chamber treatment heals wounds 75% faster than antibiotics treatment. The oxygen-rich chamber allows the cells to supply more oxygen to the wounded area and thus helps in healing.
Summary:
Management of foot ulcers consists of wound treatment and dressing the affected area to avoid infection growth and help the skin to heal.
Also Read: Sliding Scale Insulin Chart
Guidelines For Prevention & Care of Foot Ulcers
Follow the below guidelines for prevention and care from foot ulcers:
- Daily inspect your feet. Call your doctor if you notice anything like cuts, blisters, redness, swelling, or any nail problem.
- Use only lukewarm water to wash your feet. Because it relieves pain.
- Be gentle while washing your feet; carefully pat them dry, especially between the toes.
- Moisturize your feet to avoid itching or cracking, but don’t moisturize between the toes.
- Be careful while cutting nails
- Wear clean and dry socks every day.
- Don’t walk barefoot it may irritate your feet. People with diabetes should avoid walking barefoot.
- Use comfort shoes for increasing blood circulation.
- Seeing your doctor regularly is good to avoid foot complications.
Summary:
Don’t walk barefoot if diabetic and take proper foot care to avoid foot ulcers.
Avoid taking any risks when it comes to diabetic foot ulcers and other diabetes-related wounds. If you see any signs of foot infection consult your doctor immediately. The faster you receive medical advice the less are the chance of an infection.
FAQ’s:
Does a foot ulcer give a bad smell?
Is there bleeding in the foot ulcer?
There can be bleeding in foot ulcers due to serious tissue damage. Sometimes foot ulcers may discharge green or yellow fluids.
Can I get a foot ulcer if I am not diabetic?
Yes one can suffer from a foot ulcer if one does not have diabetes. The other causes of foot ulcers are improper blood circulation, leg swelling, foot deformities, nerve damage, and obesity.
How much time a diabetic foot ulcer takes to heal?
Foot ulcers can take 10 to 20 weeks to heal properly. Healing time varies from person to person due to their condition. With good medical treatment and with good blood circulation foot ulcers can be healed within 6 weeks.
Disclaimer
This site provides educational content; however, it is not a substitute for professional medical guidance. Readers should consult their healthcare professional for personalised guidance. We work hard to provide accurate and helpful information. Your well-being is important to us, and we value your feedback. To learn more, visit our editorial policy page for details on our content guidelines and the content creation process.

 English
English











